This post may refer to COVID-19
To access official information about the coronavirus, access CDC - Centers for Disease Control and Prevention.

www.yahoo.com
California becomes ground zero for holiday COVID-19 surge
California has borne the brunt of COVID-19’s deadly holiday surge. On Monday, Gov. Gavin Newsom acknowledged that the Golden State had recorded 525,000 coronavirus cases in the previous two weeks alone, with daily increases of more than 40,000 cases suddenly becoming the new norm.
Health
As the nation grapples with the latest wave of coronavirus cases, California has borne the brunt of COVID-19’s deadly holiday surge. On Monday, Gov. Gavin Newsom acknowledged that the Golden State had recorded an astonishing 525,000 coronavirus cases in the previous two weeks alone, with daily increases of more than 40,000 cases suddenly becoming the new norm.
Los Angeles County, California’s largest, is seeing the highest number of new cases. County Director of Health Services Dr. Christina Ghaly said at a news conference last week that 1 in 80 L.A. residents have been infected since the start of the pandemic.
“We’re experiencing an explosive and very deadly surge,” Los Angeles County health official Dr. Barbara Ferrer said, adding that two people are dying of COVID-19 every hour in the county.
“Over 8,000 people, who were beloved members of their families, are not coming back,” Ferrer said as she fought back tears. “And their deaths are an incalculable loss to their friends and their family, as well as our community.”
But as bad as things have become in California, health officials are also warning that the worst is yet to come.
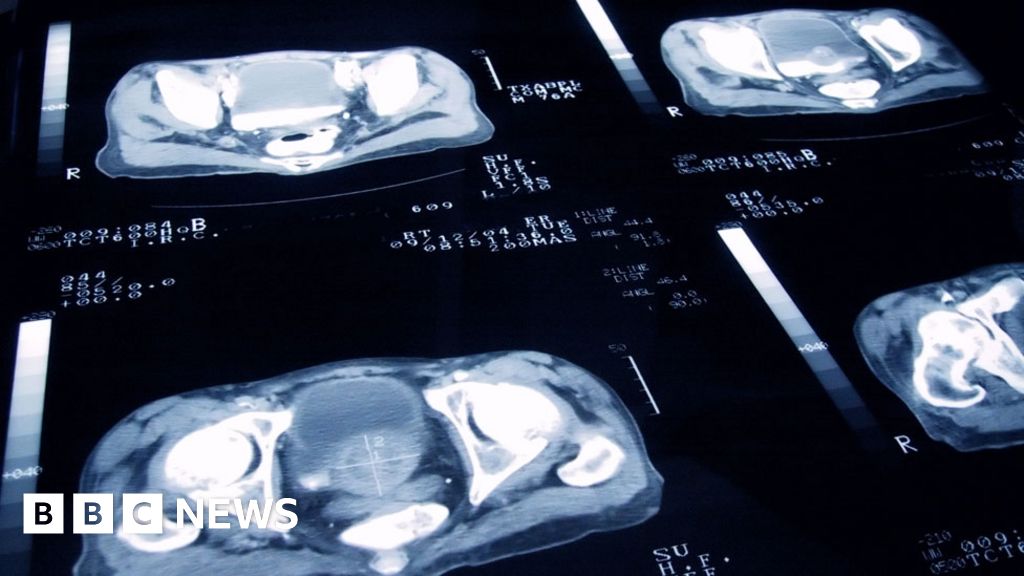
On Friday, hospitals reached a critical point that the state had worked to thwart with a stay-at-home order earlier this month, with ICU bed capacity falling to zero percent in the 11-county southern region. This encompasses Los Angeles, San Bernardino, San Diego, Ventura, Santa Barbara, San Luis Obispo, Imperial, Inyo, Orange, Riverside and Mono counties.
Cassandra Craig, a registered nurse for 10 years who works in an intensive care unit in Southern California, explained the “feeling of dread and doom” that each day on the job now brings.
“I know I’m in for something that might be sad or scary, and I know that we are bursting at the seams at our hospital way over capacity, and we just have to roll with the punches and be flexible,” Craig told Yahoo News.
Overwhelmed health systems across the state have struggled to keep up with the demands of the surge in new cases, setting up makeshift extra beds for COVID-19 patients and shopping for real estate in other parts of the hospital.
“We’ve altered rooms to accommodate ICU COVID-positive patients. We’re utilizing space in units that are not typically used for ICU. They’re used for patients who are close to going home,” Craig explained. “When you are in a space that’s not designed for critically ill COVID patients, you are limited on space, limited on materials and limited on what you can and can’t do in that room.”
On Monday, Newsom, who placed himself in precautionary quarantine for 10 days on Sunday after one of his staffers tested positive, warned that hospital staffing is extremely limited.
“We continue to see record-breaking ICU capacity, hospitals that are getting filled up, a surge that we are experiencing, not dissimilar to other parts of the country, but putting real challenges on our staffing, here in the state,” the governor said at a news conference.
Craig said that nurses are typically not allowed to have more than two patients because of a California mandate. But because of the staffing crisis, California’s medical systems have had to modify that regulation.
Craig, a mother and wife, laments the strain that the surge in cases has put on the staff. “We are working overtime. We are away from our families,” she said. “People are coming in extra. Some people are coming in on their days off. Some people are coming in for 16 hours. We are stretched thin.”
To help alleviate some of the burden, Newsom on Monday announced that the state had deployed 607 state staff, including the California National Guard, medical assistance teams, the California Health Corps, contract staff and others, in 75 facilities in 24 counties. The state has also opened alternate care sites.
According to an Associated Press report, places like Los Angeles County are also drafting emergency plans in case they have to ration lifesaving care. On Dec. 15, Newsom ordered 5,000 body bags for Southern California in preparation for what many public health experts have predicted will be a marked spike in COVID-19 deaths.
Mortality from the disease caused by exposure to the coronavirus can come quickly. Last week, Craig had a female patient in her 70s who, while not on a ventilator, was being treated with oxygen.
“Up until the end of my shift at 7:30 that night, she was awake and talking. … Very sweet lady. She died a few hours later,” Craig said, adding, “It just broke my heart that she passed away. We are sad. We are tired.”
As of Tuesday, nearly 18,000 patients in California were hospitalized due to COVID-19, more than double July’s peak of 7,170. Intensive care units are packed with 3,861 COVID-19 patients. Newsom acknowledged that a state projection model reveals that there could be nearly 100,000 hospitalizations in the next month.
While health officials believe that the rise in new infections can be traced back to October, Thanksgiving proved to be a superspreader event.
Shoni Taylor, a clinical specialist liaison at a Los Angeles hospital who supports nursing staff in her medical center, managing COVID-19-positive psych patients, expressed her grievance with Californians who have let pandemic and quarantine fatigue set in.
“It’s really frustrating when you work in health care and are on the frontlines and you see people still gathering, still having parties,” Taylor told Yahoo News, adding, “You kind of feel frustrated because ‘I’m not doing any of that. I want to go on vacation! I want to gather with all of my friends and family ... but I’m trying to be responsible.’ There’s so much resistance, and the cases are still going up and up and up.”
The recklessness of large indoor gatherings is what has helped lead to California’s most recent stay-at-home order, issued in early December, based on a region’s ICU capacity. If capacity drops below 15 percent in a designated region (Northern California, Greater Sacramento, Bay Area, San Joaquin Valley and Southern California), that area must abide by the stay-at-home order. Californians are supposed to cut down on nonessential contact outside their household unless they have to perform a necessary task like grocery shopping, picking up medication or exercise. Outdoor dining in restaurants — once seen as a silver lining for Southern California, where temperatures are expected to reach the 70s on Christmas — has also been banned, and all nonessential travel is off limits.
“Our actions today can make a difference on what happens down the road,” warned California Health and Human Services Secretary Dr. Mark Ghaly during Monday’s briefing. “Every bit of our ability to not mix [and] keep our face covering on reduce the likelihood that we either transmit COVID or ourselves are infected by someone else transmitting it to us. That becomes a victory for the state.”
Craig agreed. “Do you really want it on your conscience if somebody gets sick? It’s not worth it. It’s not worth the pain and the heartache that you’ll go through.”